Will hyperinsulinemia be better after losing weight? Why?
Hyperinsulinemia after weight loss may be caused by improper diet, insufficient exercise, side effects of drugs, abnormal metabolism, and decreased pancreatic β cell function. These factors lead to excessive stimulation of pancreatic cells, which may cause hyperinsulinemia. Therefore, treatment is needed for specific causes, such as adjusting diet structure, increasing exercise, stopping related drugs, improving metabolic abnormalities, and using insulin secretagogues. Patients are advised to seek medical treatment promptly for targeted treatment.
1. Improper eating can lead to excessive calorie intake, and the body secretes more insulin to lower blood sugar levels in order to consume excess calories. At this time, we can adjust the diet structure to reduce the intake of high-sugar and high-fat foods, and increase the ratio of dietary fiber and protein to help improve insulin sensitivity.
2. Insufficient exercise causes the body's metabolic rate to drop and requires less insulin to maintain normal blood sugar levels. It is recommended to gradually increase the time and intensity of aerobic exercise, such as brisk walking, jogging, etc., to improve cardiopulmonary function and metabolic efficiency.
3. Drug Side Effects

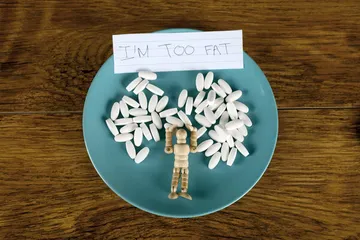
Certain weight loss drugs may reduce weight by suppressing appetite or affecting the central nervous system. These drugs may interfere with normal endocrine balance and cause hyperinsulinemia. If you find that symptoms of hyperinsulinemia occur after taking diet pills, you should immediately stop using them and consult your doctor to change to other safe and effective weight loss methods.
4. Abnormal metabolism abnormalities Autonomy metabolic abnormalities include obesity, hypertension, hyperlipidemia, etc. These factors may lead to impairment of pancreatic beta cell function, which in turn causes hyperinsulinemia. Treatment for self-metabolic abnormalities often requires a comprehensive consideration of diet, exercise and drug intervention. For example, obese patients can be managed by a combination of low-calorie diet and moderate exercise.
5. Hypofunction of islet beta cells hypofunction refers to a weakened response of the main insulin-producing cell group in the pancreas to glucose stimulation, resulting in insufficient insulin secretion. Treatment of the disease requires an individualized plan, and blood sugar levels can be controlled by oral hypoglycemic drugs or insulin injections.
In addition to the reasons mentioned above, attention should also be paid to whether there are problems such as hyperthyroidism. If necessary, relevant hormone level testing and targeted imaging examinations can be performed to detect and deal with potential health risks in a timely manner.