Will hyperinsulinemia be better after losing weight? Why

Hyperinsulinemia after weight loss may be caused by improper diet, insufficient exercise, side effects of drugs, secondary diabetes or autoimmune hypoglycemia, which lead to abnormal islet cell function. Patients are advised to adjust their diet under the guidance of their doctor, increase the amount of exercise, and avoid excessive dieting or excessive exercise to improve islet cell function.
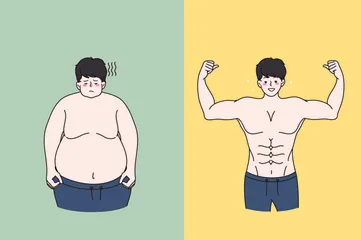
1. Improper diet leads to a decrease in calorie intake. The body reduces the metabolic rate in order to maintain normal functions, and in turn improves the utilization efficiency of carbohydrates in food by reducing insulin sensitivity. Adjusting diet and increasing exercise are the key to improving hyperinsulinemia.
2. Insufficient exercise can lead to a decrease in the ability of muscles to consume fat, which affects the body's absorption and utilization of glucose and further increases the workload of islet cells. Moderate increase in aerobic exercise such as brisk walking, running, etc. can effectively improve the body's insulin sensitivity and help restore normal levels.
3. Drug Side Effects
Certain drugs such as diuretics may interfere with the electrolyte balance in the body and indirectly affect the secretion and action of insulin. Consult your doctor before stopping relevant drugs and gradually reduce the amount to reduce discomfort.
4. Secondary diabetes Secondary diabetes is caused by other diseases that affect the function of pancreatic beta cells and lead to insufficient insulin secretion or resistance, causing hyperinsulinemia. Treatment of the primary disease is the key, such as the use of oral hypoglycemic drugs such as glibenclamide tablets and acarbose tablets to control blood sugar levels.
5. Autoimmune hypoglycemia is a disease caused by the autoimmune system mistakenly attacking pancreatic beta cells. When pancreatic beta cells are damaged, the insulin they secrete increases abnormally, causing an increase in insulin concentration in the blood. Patients need to monitor blood sugar levels regularly as prescribed and may need to bring quick supplements to deal with sudden hypoglycemic episodes.
It is recommended to regularly review fasting blood glucose, insulin release test, and C-peptide measurement to assess whether hyperinsulinemia has improved. If necessary, consider conducting genetic testing to rule out the possibility of inherited metabolic diseases.